Comprehensive combination
Our personalized immunotherapy targets the tumor without destroying healthy cells. We achieve this by combining different treatments.
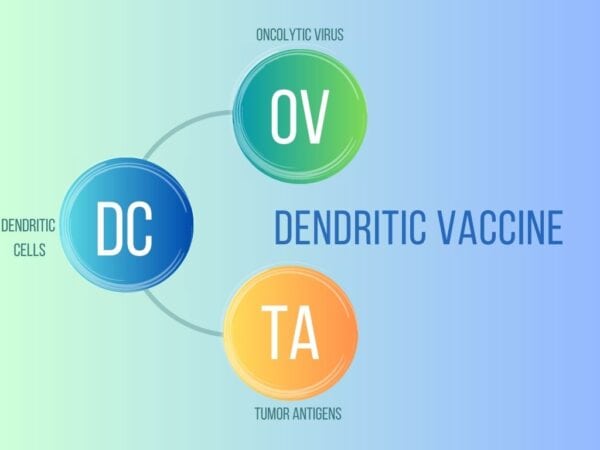
Dendritic vaccine
The basis and the most important element of our Immunotherapy is a vaccine developed by our laboratory, individually prepared for each patient. Put simply, we combine the oncolytic virus and the patient’s tumor material with the dendritic cells in our laboratory to produce a personalized vaccine. This vaccine then activates the patient’s immune system to fight the tumor. Our clinic is the only institution in Europe that has obtained regulatory approval for the production of such a vaccine.
Virotherapy
Virotherapy is an integral part of our immunotherapy. Oncolytic viruses, such as Newcastle disease virus (NDV), are viruses that attack cancer cells but are harmless to healthy cells. When the virus replicates in the cancer cells, the immune system is alerted and notices the cancer cells. As a result of viral infection, cancer cells are classified as dangerous and are attacked.
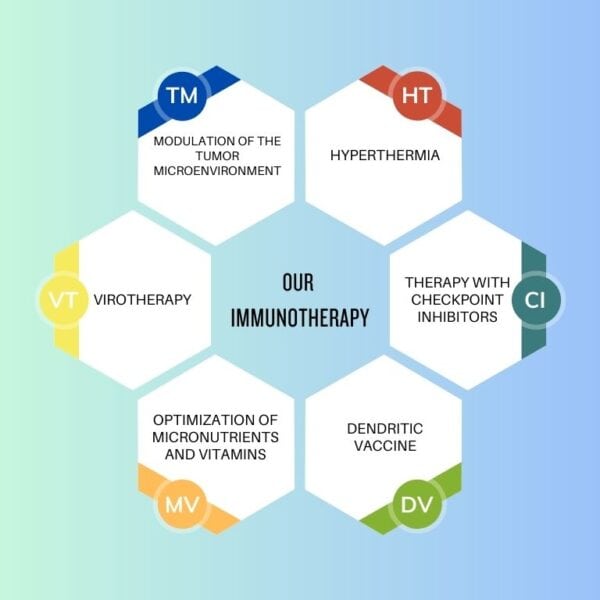
Hyperthermia
Modulated electrohyperthermia causes an increase in temperature and stimulation of cancer cells through electromagnetic waves, without affecting healthy tissue. In this way, cancer cells produce certain warning signals on their surface that provoke and intensify the immune reaction. In moderate whole-body hyperthermia, a fever-like increase in body temperature is generated under the influence of infrared light. This passive increase in temperature stimulates the immune cells responsible for fighting the tumor.
Therapy with checkpoint inhibitors
Checkpoints are the mechanisms by which the immune system is regulated from over-activation. Cancers “misuse” immune checks, also known as checkpoints, to deactivate the immune response directed against them. This is where checkpoint inhibitors come into play: they inhibit blocked signaling pathways. In a sense, they release the brakes on the immune cells and thus allow the immune system to fight the tumor again. However, PD-1 checkpoint inhibitors are only effective when an immune response against the tumor is already in place.
Tumor microenvironment modulation
The tumor microenvironment refers to the connective tissue structure in which the tumor is embedded. There is a direct interaction between this tissue and cancer cells, which affects the growth of cancer cells and the effectiveness of immunotherapy. Hence, our immunotherapy takes into account and modulates the tumor microenvironment.
Optimization of micronutrients and vitamins
For the immune system to function optimally, it must be supplied with the right amount of microelements and vitamins. We give them specifically to optimize the immune response when needed.
Dendritic vaccine
Unmasking cancer cells and effectively fighting them
Through the repeated use of our vaccine, the patient’s immune system is activated and allows the camouflage mechanisms of the cancer cells to be detected and acted upon. The key role here is played by dendritic cells acting as messengers and a virus that is not harmful to humans. As with regular vaccines, the immune system can build an immune memory against tumor antigens, thus ensuring long-term effectiveness.

Components of a personalized vaccine
Using viruses against cancer
Some oncolytic viruses can multiply only in cancer cells, destroying them in the process, while healthy cells can defend themselves against the virus. Newcastle disease virus (NDV) is such a virus. It is completely harmless to humans: it multiplies only in human cancer cells, without damaging healthy cells. Infected cancer cells send out warning signals that alert and activate the immune system. In this way, Newcastle virus increases the effectiveness of our vaccine.

Vaccine production
The first step is to take a blood sample from the patient. In our laboratory, monocytes, a type of white blood cell, are isolated and grown into dendritic cells. They are matured in the lab and contain information about tumor components and viral threat signals. After vaccination, dendritic cells present tumor-specific molecules to the patient’s immune system and thus activate T cells. The role of T cells is to destroy diseased cells. Thanks to the information the T cells have received, they can now recognize and attack cancer cells throughout the body.
The principle of dendritic cell vaccination, on which our vaccine is based, has been the subject of intensive research for several years. The first approved drug of this type is Provenge (Sipuleucel T) against prostate cancer. This, however, does not use the patient’s own tumor material, but uses pre-selected antigens. At an advanced stage of clinical trials, another vaccine (DC-Vax) has shown promising results but has not yet been approved. This vaccine also uses dendritic cells loaded with tumor lysate from the patient. However, it does not contain an oncolytic virus to increase its effectiveness.
